Navigating the Complexities of Employer-Sponsored Health Insurance Claims: A Comprehensive Guide
Related Articles: Navigating the Complexities of Employer-Sponsored Health Insurance Claims: A Comprehensive Guide
Introduction
With great pleasure, we will explore the intriguing topic related to Navigating the Complexities of Employer-Sponsored Health Insurance Claims: A Comprehensive Guide. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
Navigating the Complexities of Employer-Sponsored Health Insurance Claims: A Comprehensive Guide
Navigating the healthcare system, particularly when it comes to insurance claims, can be a daunting task for individuals and employers alike. Employer-sponsored health insurance plans offer a valuable benefit to employees, providing access to medical care and financial protection. However, understanding the process of filing and processing claims, especially in cases where the claim involves a pre-existing condition or a complex medical procedure, can be challenging. This comprehensive guide aims to shed light on the intricacies of employer-sponsored health insurance claims, providing clarity and guidance for both employees and employers.
Understanding the Basics of Employer-Sponsored Health Insurance
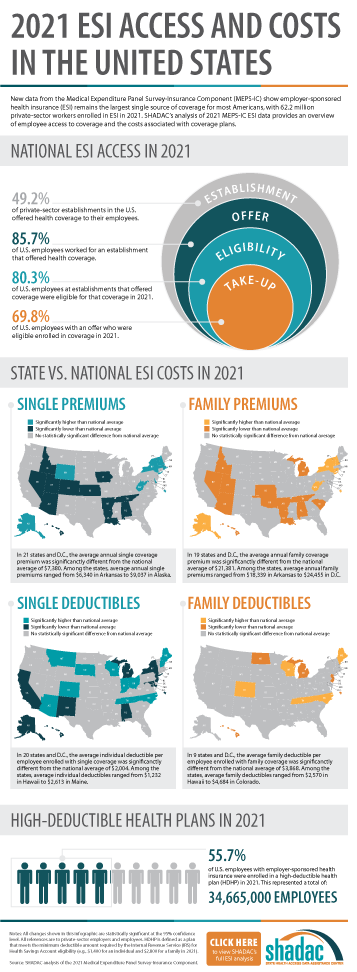
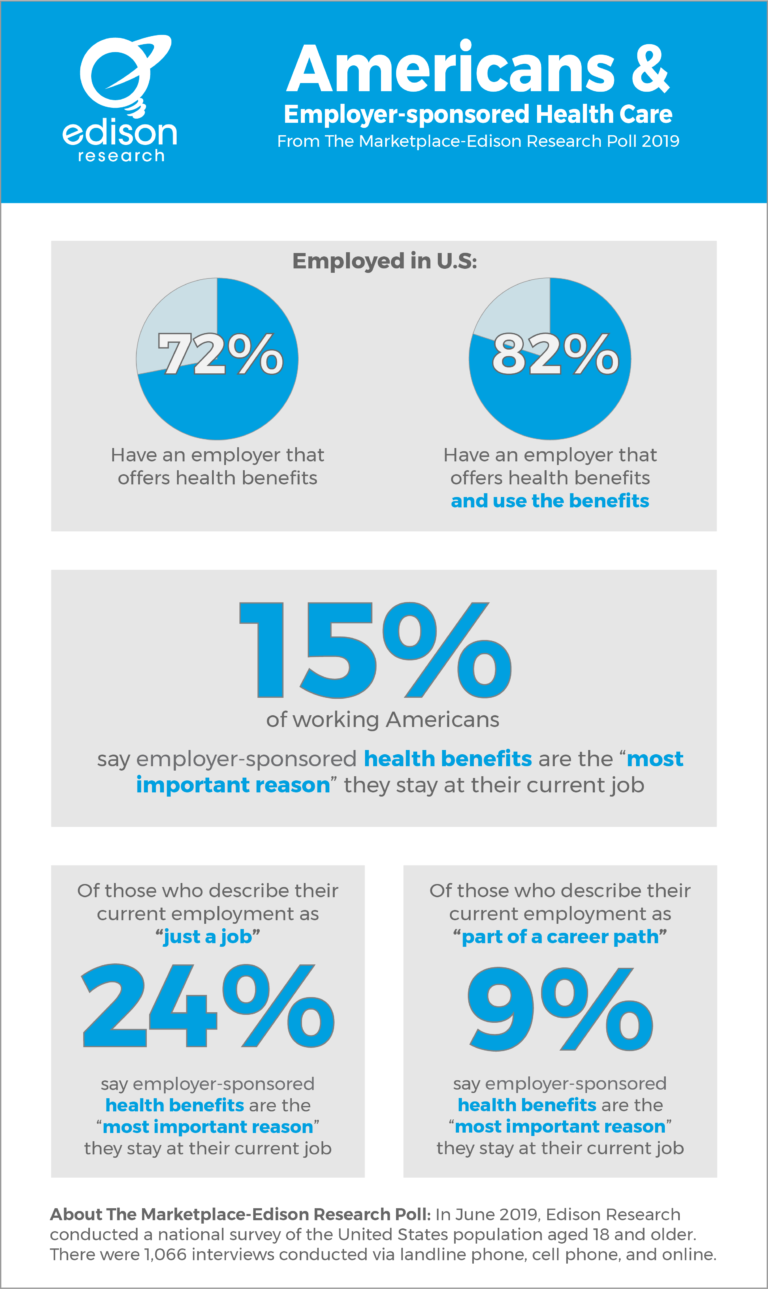
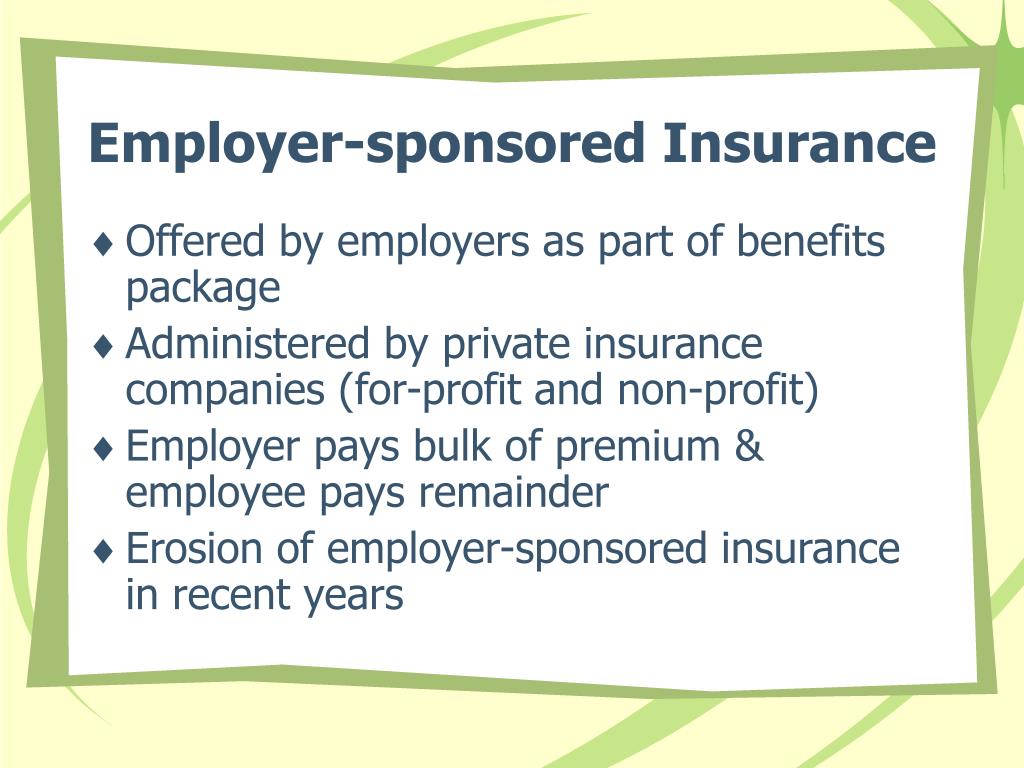
Employer-sponsored health insurance plans are typically offered through group health insurance policies, where the employer acts as the policyholder and the employees are the beneficiaries. These plans can vary significantly in coverage, benefits, and costs, depending on factors such as the size of the employer, industry, and geographic location.
The Role of the Employer
Employers play a crucial role in the administration of health insurance plans. They are responsible for:
- Selecting and negotiating with insurance carriers: Employers carefully evaluate different insurance plans and negotiate terms with carriers to secure the best coverage for their employees at a reasonable cost.
- Administering the plan: Employers handle the day-to-day operations of the plan, including enrollment, premium collection, and claim processing.
- Providing information and resources to employees: Employers are responsible for educating employees about their benefits, plan details, and the claims process.
The Role of the Employee
Employees are the beneficiaries of employer-sponsored health insurance plans. Their responsibilities include:
- Understanding their coverage: Employees should be familiar with their plan’s benefits, limitations, and procedures.
- Choosing a primary care physician (PCP): Most plans require employees to select a PCP who serves as their primary point of contact for healthcare needs.
- Filing claims: Employees are responsible for submitting claims for medical services received, ensuring accurate and complete documentation.
The Claims Process: A Step-by-Step Guide
The claims process typically involves the following steps:
- Receiving medical care: Employees receive medical services from their PCP or other authorized healthcare providers.
- Obtaining a claim form: Employees can request claim forms from their insurance carrier or download them online.
- Completing the claim form: Employees must accurately fill out the claim form, providing all necessary information, including the date of service, the medical provider’s details, and the nature of the medical service.
- Submitting the claim: Employees submit the completed claim form to the insurance carrier, either by mail, fax, or online.
- Claim processing: The insurance carrier reviews the claim, verifies the information, and determines the amount of coverage.
- Payment: The insurance carrier sends payment to the medical provider, or directly to the employee in some cases.
Common Claim Issues and Resolutions
While the claims process is generally straightforward, certain situations can lead to complications:
- Pre-existing conditions: Conditions that existed before the insurance policy’s effective date may be subject to limitations or exclusions.
- Complex medical procedures: Claims for complex surgeries, treatments, or diagnostic tests may require additional documentation and approval.
- Out-of-network providers: Seeking care from providers outside the plan’s network can lead to higher out-of-pocket expenses.
- Claim denials: Claims may be denied for various reasons, including missing information, incorrect coding, or lack of authorization.
Tips for Successful Claim Filing
- Keep accurate records: Maintain detailed records of all medical services received, including dates, providers, and costs.
- Understand your coverage: Familiarize yourself with your plan’s benefits, limitations, and procedures.
- Seek pre-authorization: For complex procedures, obtain pre-authorization from the insurance carrier before receiving treatment.
- File claims promptly: Submit claims within the stipulated timeframe to avoid delays.
- Follow up on claims: Track the status of your claims and contact the insurance carrier if there are any issues.
FAQs: Addressing Common Concerns
Q: What happens if my claim is denied?
A: If your claim is denied, you will receive a written explanation outlining the reasons for the denial. You have the right to appeal the decision and provide additional information or documentation.
Q: What are the different types of health insurance plans?
A: Common types include:
- Health Maintenance Organization (HMO): Offers a network of providers and requires a primary care physician referral for specialist visits.
- Preferred Provider Organization (PPO): Provides greater flexibility in choosing providers, with higher costs for out-of-network care.
- Point of Service (POS): Combines elements of HMO and PPO, offering network and out-of-network options with varying costs.
Q: What is a deductible?
A: A deductible is the amount you must pay out-of-pocket before your insurance coverage begins.
Q: What is coinsurance?
A: Coinsurance is the percentage of medical costs you share with the insurance company after the deductible is met.
Q: What is a co-pay?
A: A co-pay is a fixed amount you pay for specific medical services, such as doctor’s visits or prescriptions.
Conclusion
Navigating employer-sponsored health insurance claims can be a complex process, but with a clear understanding of the procedures, benefits, and common issues, employees and employers can ensure a smooth and efficient experience. By actively engaging with their insurance plans, employees can maximize their benefits and access the healthcare they need. Employers, in turn, can foster a healthy and productive workforce by providing clear communication, resources, and support to their employees regarding their health insurance benefits.





Closure
Thus, we hope this article has provided valuable insights into Navigating the Complexities of Employer-Sponsored Health Insurance Claims: A Comprehensive Guide. We hope you find this article informative and beneficial. See you in our next article!